This minimises the need for repeated surgery and optimises your chance of a long-term cure.
The priority for your skin cancer removal
The priority for skin cancer removal is to ensure the skin cancer is completely removed. This is partly why we target such a low incomplete excision rate of less than 0.1%. This is far lower than the norm of 5-10% (some studies suggest it is as high as 20%). A low incomplete excision rate also contributes to a low risk of the skin cancer coming back (recurrence).
Unfortunately, many skin cancers have very subtle borders, sometimes making it extremely difficult to determine the edge of a skin cancer.
Extremely Low Incomplete Excision Rates
At Skintel, we have a history of extremely low incomplete excision rates.
This means that at Skintel, you are more likely to:
- Have your skin cancer treated successfully on the first attempt.
- Avoid repeated surgery for the same skin cancer.
- Achieve better results.
Skin cancer removal options
In some situations, minimally invasive treatments may be an option. This is particularly the case for very early or superficial skin cancers. Sometimes we can treat these skin cancers with a cream.
We will discuss these options with you when appropriate:
- Efudix treatment.
- Aldara treatment.
- Photodynamic Therapy (PDT).
- Cryotherapy (Liquid Nitrogen treatment).
- Curettage & Electrodessictaion.
- Punch excision.
- Shave excision.
- Surgical excision.
- Mohs Surgery – when the cancer is on the face, head, neck or in difficult sites.
Good cosmesis
While complete removal of skin cancer should be the priority in most cases, this does not mean that a good cosmetic outcome is neglected. On the contrary, we ensure we optimise the cosmetic outcome. Nonetheless, skin cancer removal is a balance between adequate removal of the cancer against functional and cosmetic outcomes.
During the planning stage, we will discuss what will be done to ensure you are happy with the outcome.
Surgical excision for skin cancer removal
An excision is performed with local anaesthetic to remove the lesion which is normally sent to the laboratory for analysis. The wound is then stitched together and requires you to rest to optimise the healing process.
We will add a safety margin which is often 4-6 mm wide, although deep melanomas may need to be as wide as 2 cm. An excision with a wide margin is referred to as a wide local excision (WLE). Normally the wound is elongated and pulled together to create a flat, straight wound (direct closure). However, in some situations, we may need to undertake different closure methods to optimise the cosmetic result. These can include:
- Flaps: this involves recruiting adjacent skin into the wound while minimising the distortion of adjacent structures. Sometimes we use flaps to allow us to hide as much of the scar line as possible such as within the hairline or in natural creases. This may result in scar lines that are curved or angular shapes.
- Split-thickness skin grafts: involve taking a superficial layer of skin from a distant site and stitching this into the wound. These types of grafts will normally heal with a depressed scar.
- Full-thickness skin grafts: involve taking a full-thickness piece of skin from a distant site and stitching this into the wound. Full-thickness grafts can often heal with good cosmetic results if a good tissue texture match can be obtained from the donor site.
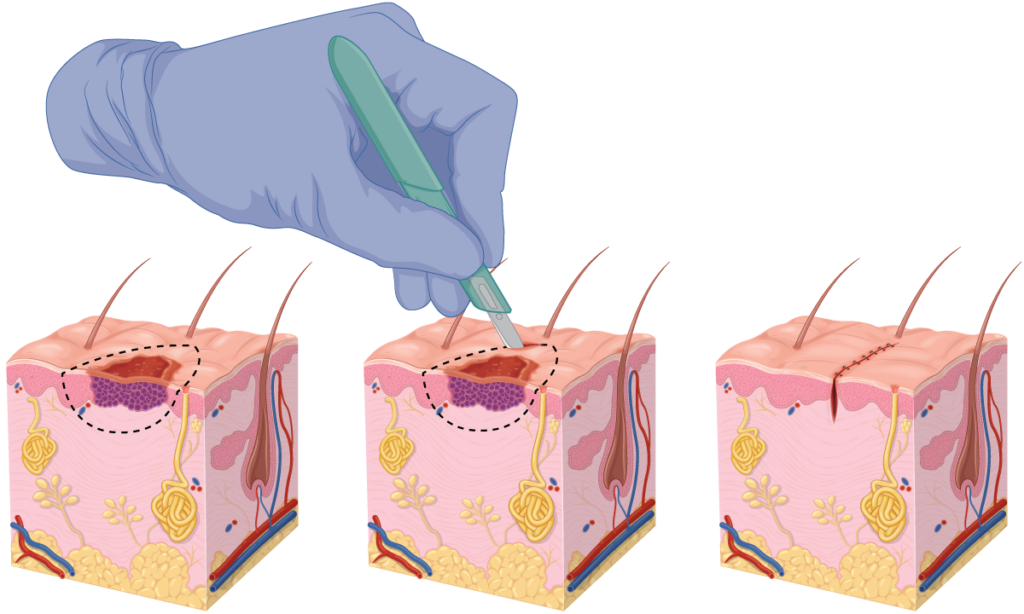
The procedure
- While it really should go without saying, we cannot emphasise enough that the most critical step is identifying skin cancer and where it transitions to normal skin (the margin). A safety margin will be added to this, which is normally 4-6 mm wide.
- The surgery will then be planned out to achieve a good cosmetic outcome. All of this will involve drawing on the skin with a felt pen and you are more than welcome to inspect the plan and ask questions.
- Local anaesthetic will be infiltrated into the surgical site.
- The excision will be carried out which may involve undermining to free up the tissues and strengthen the wound.
- Electrocoagulation may be used to stop bleeding. This helps to minimise the risk of complications and improve the cosmetic result.
- The wound will be stitched, normally using two layers of sutures. The deep layer uses a dissolving suture that provides structural support to the wound to reduce the risk of the wound stretching (dehiscing). The superficial layer can use either a dissolving or non-dissolving suture and helps provide a good cosmetic outcome.
- The wound will be cleaned and a dressing applied.
- The specimen will be sent to the laboratory for histological analysis.
- You will be provided with a written information sheet that includes our after-hours contact number. While we don’t expect problems, we want to ensure that we are there for you should the unexpected arise.
Post-procedure
After the procedure has been completed, we will not abandon you.
We will discuss how the surgery went and you will even be given an opportunity to inspect our work – we take pride in our work and have nothing to hide. Although, we appreciate that some people would rather not look immediately after surgery. We will give you aftercare information and dressings to go home with after your procedure.
While we provide a good cosmetic outcome at the end of surgery, wound healing is a team effort. It is important for you to rest after the procedure to ensure that tension on the wound is minimised. This will allow the wound to heal with a good result. We encourage you to plan your procedure so that you can take things easy for about one week following surgery.
It will normally take 1-3 weeks for the laboratory to issue the histology report. We routinely ensure that your GP is notified of these results, however, please advise us if you prefer we don’t send the results to your GP.
Why should I have my procedure at Skintel?
We take pride in good outcomes for patients and ensure that we provide the best cosmetic outcome possible. This is why the majority of our patients return time and again for further care.
References
- Bangash, HK. Ibrahimi, OA. Lawrence, JG. et. al. Who Do You Prefer? A Study of Public Preferences for Health Care Provider Type in Performing Cutaneous Surgery and Cosmetic Procedures in the United States. Dermatol Surg. 2014;40(6):671-8. doi: 10.1111/dsu.0000000000000016

