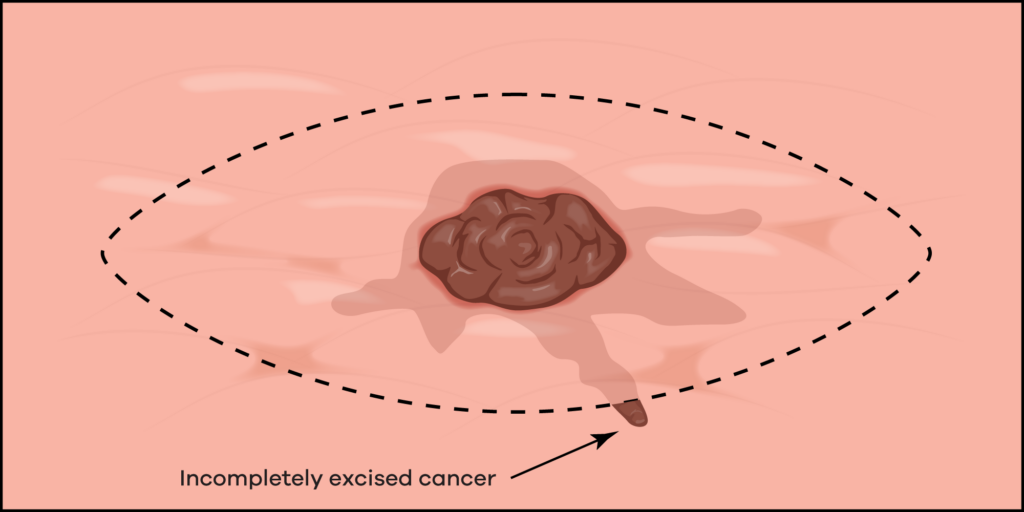
This remnant skin cancer can continue to grow silently until it either appears on the surface of the skin again or starts to cause problems with other structures.
It is an important concept to understand as it is often not well understood, and neither are the consequences.
The best cure rate is achieved when the skin cancer is cut out completely the first time.
What happens during surgery?
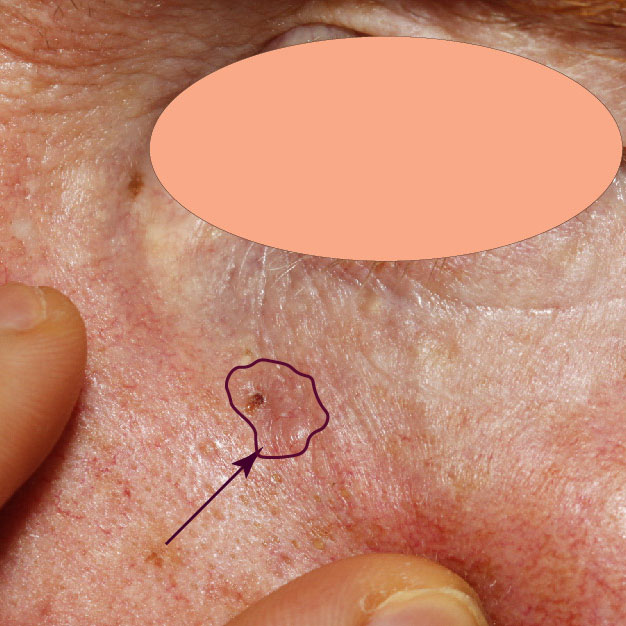
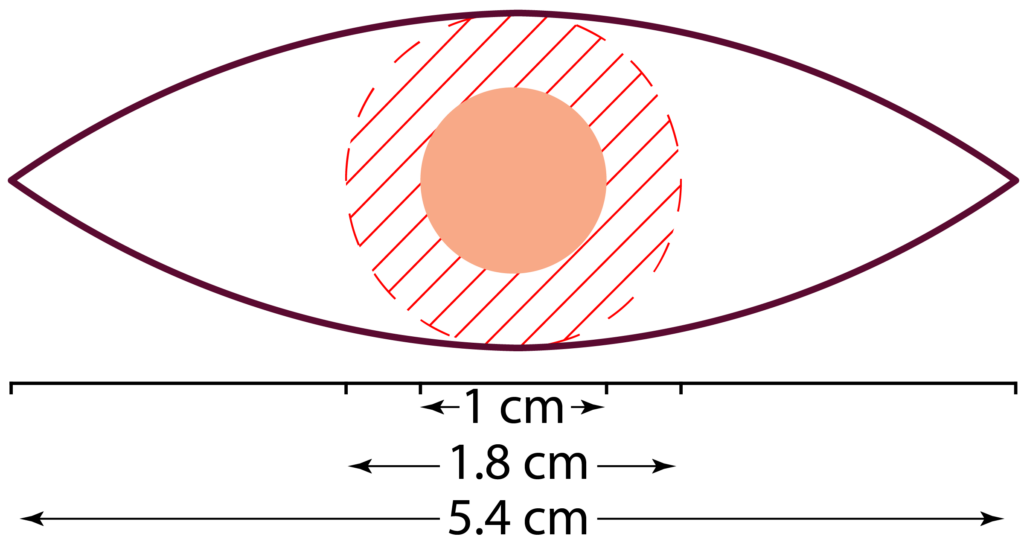
During the planning of a wide local excision (WLE), a key step is the surgeon’s ability to identify the edge of the skin cancer and where it transitions to normal skin. The difficulty is that this edge can be a challenge to identify. However, once this edge has been identified a safety margin of 4-6 mm is added and then this is converted into an ellipse that marks out the incision line.
Of course, if the edge of the skin cancer is not identified correctly, then the surgeon may cut right through the skin cancer leaving residual skin cancer in the body.

The 4-5 mm margin has been a long-accepted practice and was ‘validated’ by a meta-analysis published in 2010 that looked at recurrence rates of BCCs against the surgical margins taken at the time of surgery. Shockingly, the study included an average incomplete excision rate of 14% with a range of up to 55% which makes drawing conclusions flimsy. Nonetheless, they did observe a trend of increased recurrence rates with decreasing surgical (safety) margins.
Regardless, the current accepted practice is to take at least a 4 mm margin for BCCs and this results in the observed recurrence rates of 5-15%. Recommendations for higher-risk lesions are in the ballpark of 4-6 mm margins. Melanomas may need up to a 20 mm margin – again this is determined by the risk profile of the particular melanoma, which you can read about on our melanoma page.
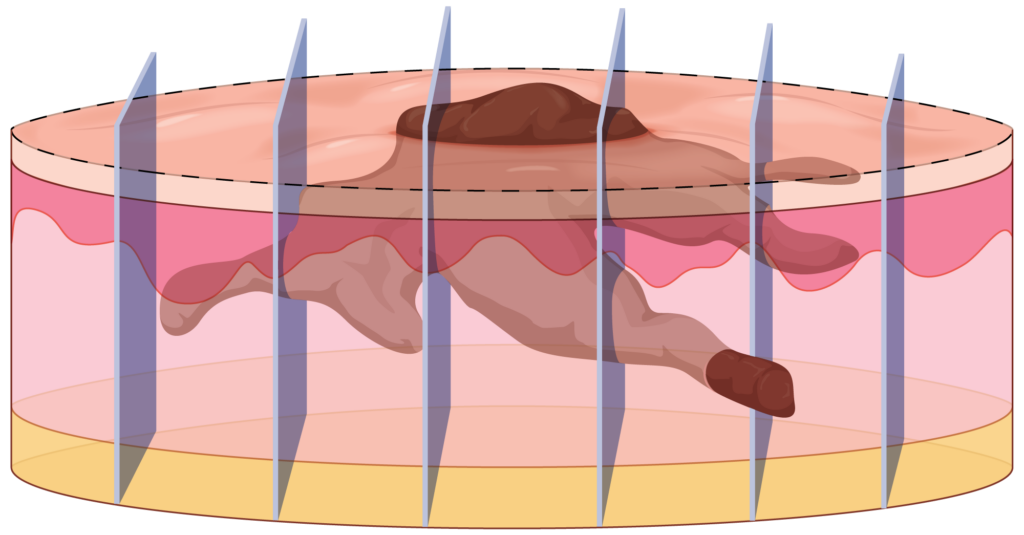
How are surgical specimens processed?
Once removed from the body, the specimen is sent to the laboratory where it is fixed in formalin. The specimen is then cut into slices like a loaf of bread (referred to as bread loafing). However, typically less than 5% of the specimen is selected for staining and preparation for these sections to be mounted on slides. The slides are then reviewed by the pathologist.
In our bread-loaf analogy, this would be similar to only looking at three slices out of a loaf of bread. Of course, this introduces uncertainty regarding the validity of the histology report.
Does a negative margin mean the cancer has been removed?
Not necessarily.
While a negative margin on the pathology report is usually assumed to mean a complete excision, all it means is that there was no tumour seen at the surgical margin in the few sections reviewed by the pathologist.
Incidentally, this uncertainty is one of the arguments for Mohs surgery which analyses the complete surgical margin and more accurately determines whether the cancer was completely excised.
What is the implication of an incomplete excision?
Not all incompletely excised skin cancers come back (recur). Studies have demonstrated that about 25-40% of reported incompletely excised BCCs will recur if left alone. However, many people are uncomfortable with the idea of leaving a ticking timebomb alone so will usually proceed to a re-excision. Unfortunately, recurrent skin cancers can be larger and more complicated to remove when they recur.
Does an incomplete excision rate influence the recurrence rate?
The incomplete excision rate is the number of reported incomplete excisions out of all the skin cancers removed during that period. So, for example, if there were 5 incomplete excisions for 100 skin cancers removed, then the incomplete excision rate would be 5%. It is important to note that, due to the uncertainty around pathology reporting of clear surgical margins, the actual incomplete excision rate will be higher than the reported incomplete excision rate.
Unfortunately, it is impossible to know what the true incomplete excision rate is. Other than a surgeon’s ability, there are some factors that will impact incomplete excision rates: high risk and larger lesions will inevitably result in a higher incomplete excision rate.
What is an acceptable reported incomplete excision rate?
We consider the incomplete excision rate to be one of the few key performance indicators (KPI) for skin cancer removal surgery. New Zealand studies have found that the incomplete excision rate for dermatologists is around 0.5% on average. Broader studies have found incomplete excision rates of up to 20% for some doctors.
We personally target a reported incomplete excision rate of less than 0.1%, or 1 in 1,000 skin cancers. Internally, we set a threshold of 0.3% that prompts a formal performance review when any of our doctors breach this level. This threshold is in line with the performance of other dermatologists as reported in the literature and is well below the industry standard level of about 5-10%. If you are interested, the full results of this study are available on the website of the British Journal of Dermatology.
We believe a low incomplete excision rate also indicates that the doctor is capable of reliably finding skin cancers during skin checks as it demonstrates a heightened ability to detect subtle and early changes of skin cancer.
Shouldn’t you be measuring recurrence rates?
Ideally yes, this would be a better measure of a patient’s real-world outcomes. However, there is a significant time delay (up to 5-10 years) for recurrences to develop. People may have changed doctors or doctors may have moved elsewhere over that time period making it difficult to audit and track recurrence rates accurately. In contrast, using a proxy like incomplete excision rates, we can collate more accurate data in a timely manner as the pathology reports are normally issued within four weeks.
References
- Gulleth Y, Goldberg N, Silverman RP, Gastman BR. What is the best surgical margin for a Basal cell carcinoma: a meta-analysis of the literature. Plast Reconstr Surg 2010; 126:1222. doi: 10.1097/PRS.0b013e3181ea450d
- Salmon, P., Mortimer, N., Rademaker, M., Adams, L., Stanway, A., & Hill, S. (2010). Surgical excision of skin cancer: the importance of training. British Journal of Dermatology, 162(1); 117:122. doi: 10.1111/j.1365-2133.2009.09548.x
- Jarrett PR, Salmon PJM. Carcinomas in the Bay of Plenty: incomplete excision rates [Letter]. NZ Med J2006; 119: U1811.

